India Healthcare Claims Management Market Outlook to 2030
Region:Asia
Author(s):Meenakshi Bisht
Product Code:KROD7294
November 2024
95
About the Report
India Healthcare Claims Management Market Overview
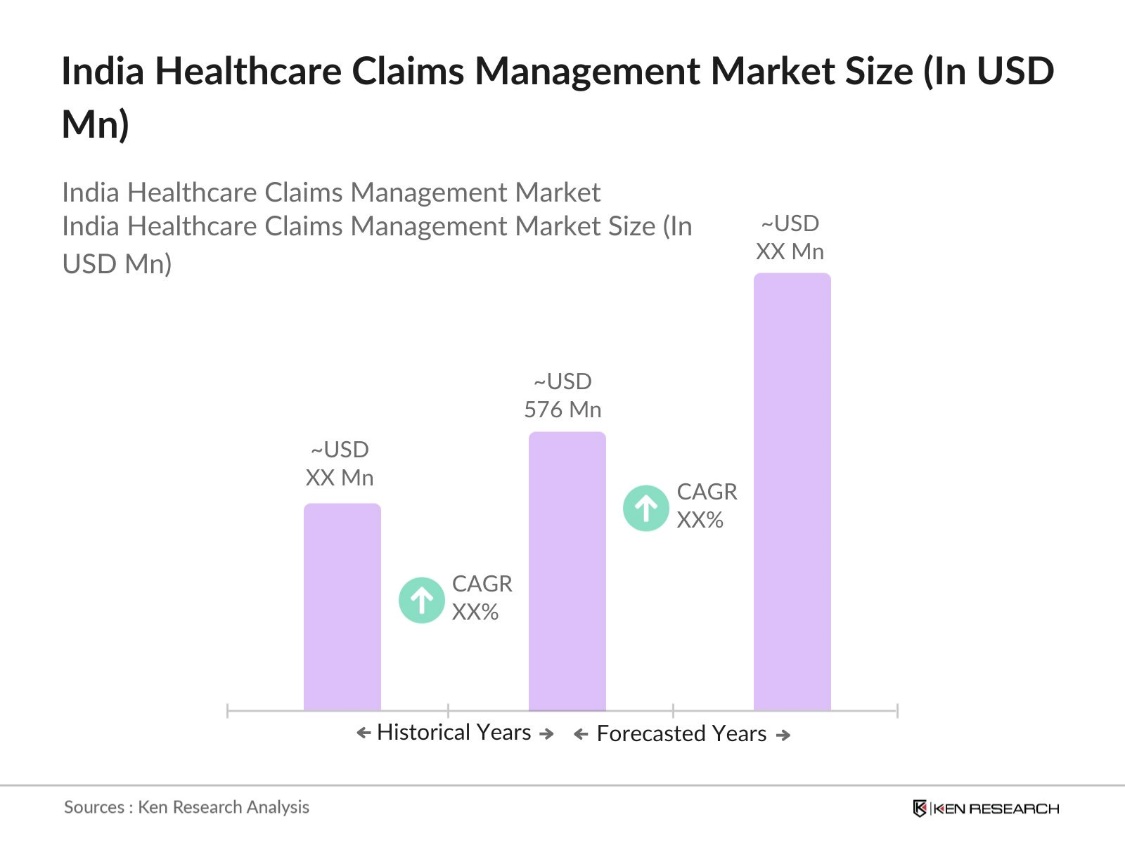
- The India healthcare claims management market was valued at USD 576 million, driven by the increasing adoption of health insurance and advancements in digital technologies. This expansion is primarily due to the rising penetration of health insurance, government initiatives promoting digital healthcare solutions, and the need for efficient claims processing systems.
- Major metropolitan areas such as Delhi, Mumbai, and Bengaluru dominate the healthcare claims management market in India. These cities have a high concentration of healthcare providers, insurance companies, and technology firms, facilitating the adoption of advanced claims management solutions. Additionally, the higher awareness and demand for health insurance products in these urban centers contribute to their market dominance.
- Indias data localization mandates require storing healthcare data within the country to ensure security and privacy. Enforced through the 2023 Data Protection Bill, healthcare providers have complied, allowing for more secure claims processing and record-keeping, supporting a safer claims management environment.
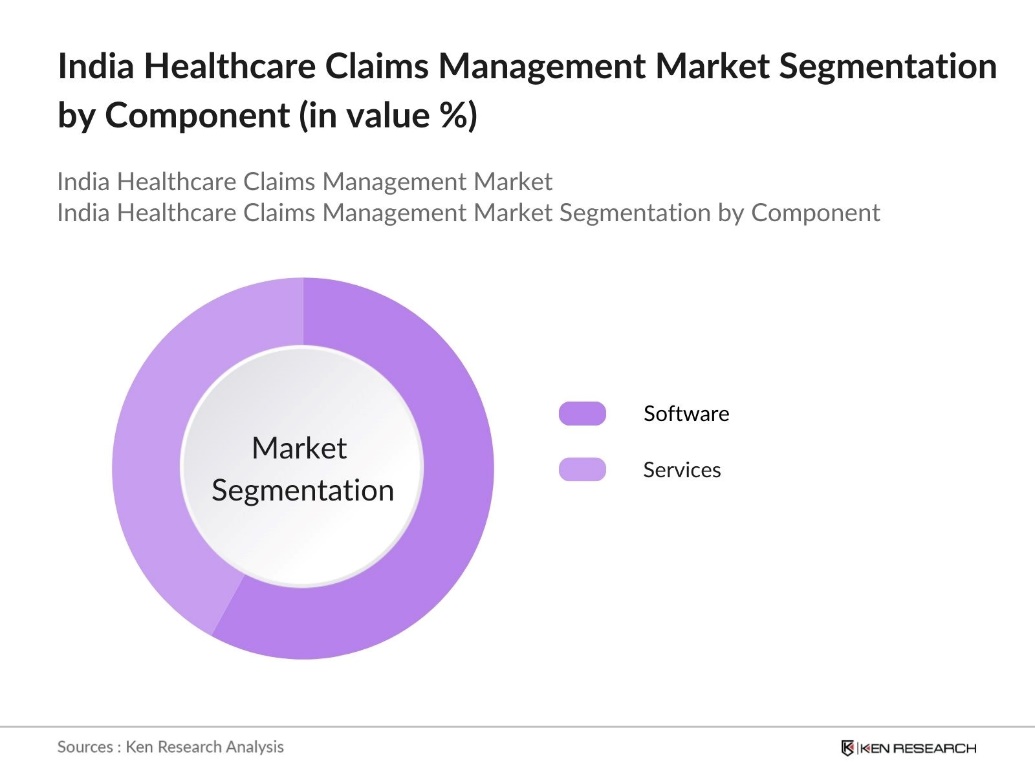
India Healthcare Claims Management Market Segmentation
By Component: The market is segmented by component into software and services. The software segment holds a dominant market share due to the increasing need for automated solutions that streamline claims processing, reduce errors, and enhance operational efficiency. Healthcare providers and insurers are investing in robust software platforms to manage the growing volume of claims efficiently.
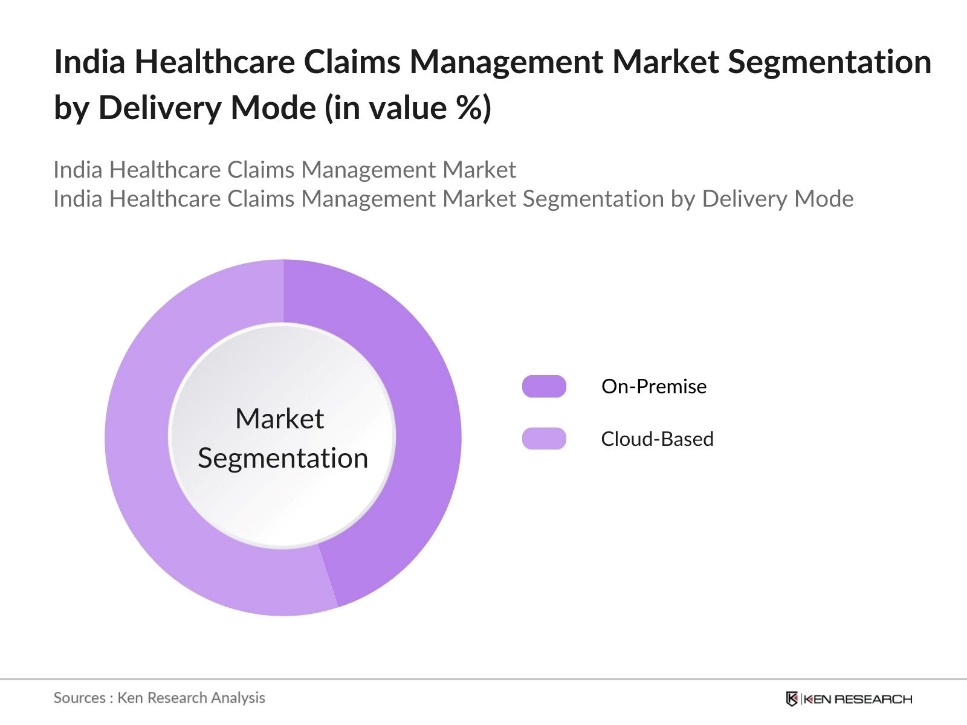
By Delivery Mode: The market is segmented by delivery mode into on-premise and cloud-based solutions. Cloud-based solutions are gaining a larger market share due to their scalability, cost-effectiveness, and ease of access. The flexibility offered by cloud-based platforms allows healthcare organizations to manage claims data securely and efficiently, without the need for significant upfront infrastructure investments.
India Healthcare Claims Management Market Competitive Landscape
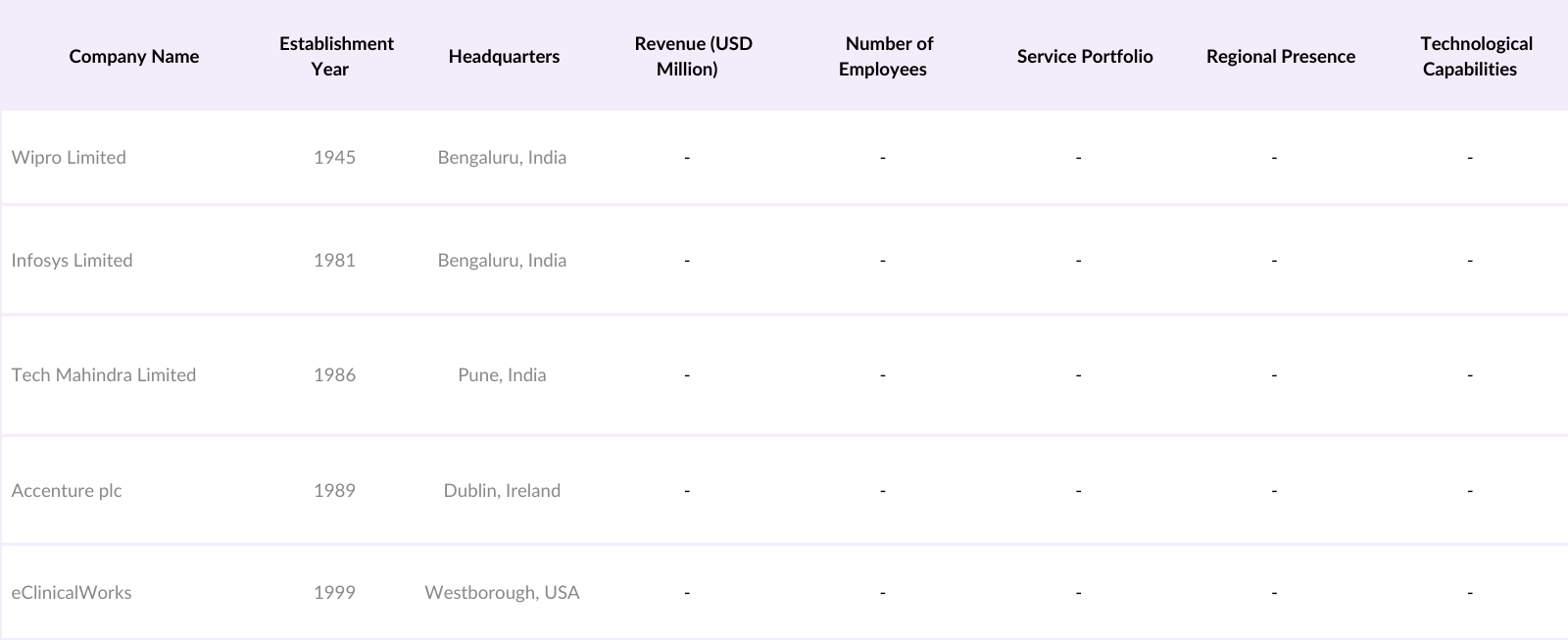
The India healthcare claims management market is characterized by the presence of several key players offering a range of solutions and services. These companies are focusing on technological advancements, strategic partnerships, and expanding their service portfolios to strengthen their market position.
India Healthcare Claims Management Industry Analysis
Growth Drivers
- Increasing Health Insurance Penetration: India has seen a notable increase in health insurance enrollment, driven by government programs and heightened health awareness. As of 2023, over 500 million individuals are covered under various health insurance schemes, such as the Ayushman Bharat scheme, which provides financial protection to low-income families Additionally, the Indian government's expenditure on healthcare has further supporting insurance penetration and enhancing claims management processes.
- Adoption of Digital Technologies: India's digital infrastructure has rapidly evolved, with over 850 million internet users as of 2024. This digital surge has enabled the adoption of digital healthcare solutions, including claims management, where the integration of digital records, AI-driven processing, and mobile apps is optimizing claims efficiency. Government-backed digital initiatives like the National Digital Health Mission have created a digital framework for managing patient records, fostering easier claims verification and reducing fraud risk.
- Rising Incidence of Healthcare Frauds: Healthcare fraud presents a significant financial challenge in the Indian insurance sector, with a high incidence of fraudulent claims, including inflated bills and false treatments. This rise in fraud cases has increased the demand for advanced claims management systems to ensure authenticity and transparency. As a result, there is a growing emphasis on implementing secure, data-driven claims management solutions to detect and mitigate these issues, helping insurers manage financial risks and maintain service integrity in the healthcare ecosystem.
Market Challenges
- High Implementation Costs: Digital claims management systems require substantial investments in technological infrastructure and cybersecurity, leading to high implementation costs. These expenses create financial barriers, particularly for smaller healthcare providers, limiting their capacity to adopt these technologies fully. As a result, the adoption pace of digital claims management solutions across the healthcare sector remains uneven, with larger institutions better positioned to bear the costs compared to smaller facilities.
- Data Privacy and Security Concerns: Data privacy and security are critical challenges in healthcare claims management, with significant volumes of sensitive information being handled daily. Recent regulatory measures have introduced stringent guidelines to protect personal data, but compliance can be costly and complex to implement. This challenge places an additional burden on healthcare providers, requiring investments in secure practices and infrastructure to safeguard data and maintain compliance, thus impacting the scalability and effectiveness of digital claims management solutions.
India Healthcare Claims Management Market Future Outlook
Over the next five years, the India healthcare claims management market is expected to witness substantial growth, driven by continuous government support, technological advancements, and increasing demand for efficient healthcare services. The implementation of national health schemes and the push towards digital healthcare ecosystems will further propel the adoption of advanced claims management solutions. Additionally, the growing awareness among consumers regarding health insurance benefits is anticipated to contribute to market expansion.
Market Opportunities
- Technological Advancements: Technological advancements, especially in AI and blockchain, are transforming claims processing in India's healthcare sector. These technologies improve accuracy by enabling automated verification and advanced fraud detection, helping reduce errors and streamline claims approval. Government initiatives promoting AI and digital solutions further support the integration of such technologies in claims management, creating a robust, tech-enabled ecosystem that enhances efficiency and reliability in processing healthcare claims.
- Expansion into Rural Markets: With a large portion of Indias rural population underserved by health insurance, there is a significant opportunity to expand claims management services into these areas. Government programs focused on rural healthcare access encourage the deployment of claims management systems that can efficiently handle claims from these regions. Simplified digital platforms tailored for rural populations make it easier to integrate these communities into the formal healthcare system, enabling faster, more accessible claims processing and improving overall healthcare reach.
Scope of the Report
|
Component |
Software |
|
Type |
Integrated Solutions |
|
Delivery Mode |
On-Premise |
|
End-User |
Healthcare Payers |
|
Region |
North West |
Products
Key Target Audience
Health Insurance Companies
Healthcare IT Industry
Medical Billing and Coding Companies
Government and Regulatory Bodies (e.g., Insurance Regulatory and Development Authority of India)
Investors and Venture Capitalist Firms
Banks and Financial Institutions
Companies
Players Mentioned in the Report
Wipro Limited
Infosys Limited
Tech Mahindra Limited
Accenture plc
eClinicalWorks
Cognizant Technology Solutions
Tata Consultancy Services
IBM India Pvt. Ltd.
Oracle India Pvt. Ltd.
Cerner Corporation
Table of Contents
1. India Healthcare Claims Management Market Overview
1.1. Definition and Scope
1.2. Market Taxonomy
1.3. Market Growth Rate
1.4. Market Segmentation Overview
2. India Healthcare Claims Management Market Size (In USD Mn)
2.1. Historical Market Size
2.2. Year-On-Year Growth Analysis
2.3. Key Market Developments and Milestones
3.India Healthcare Claims Management Market Analysis
3.1. Growth Drivers
3.1.1. Increasing Health Insurance Penetration
3.1.2. Adoption of Digital Technologies
3.1.3. Government Initiatives and Policies
3.1.4. Rising Incidence of Healthcare Frauds
3.2. Market Challenges
3.2.1. High Implementation Costs
3.2.2. Data Privacy and Security Concerns
3.2.3. Lack of Skilled Workforce
3.3. Opportunities
3.3.1. Technological Advancements
3.3.2. Expansion into Rural Markets
3.3.3. Public-Private Partnerships
3.4. Trends
3.4.1. Integration of AI and Machine Learning
3.4.2. Cloud-Based Solutions Adoption
3.4.3. Emphasis on Fraud Detection Mechanisms
3.5. Government Regulations
3.5.1. Health Insurance Portability and Accountability Act (HIPAA) Compliance
3.5.2. Data Localization Norms
3.5.3. Ayushman Bharat Scheme Implications
3.6. SWOT Analysis
3.7. Stakeholder Ecosystem
3.8. Porters Five Forces Analysis
3.9. Competitive Landscape
4. India Healthcare Claims Management Market Segmentation
4.1. By Component (In Value %)
4.1.1. Software
4.1.2. Services
4.2. By Type (In Value %)
4.2.1. Integrated Solutions
4.2.2. Standalone Solutions
4.3. By Delivery Mode (In Value %)
4.3.1. On-Premise
4.3.2. Cloud-Based
4.4. By End-User (In Value %)
4.4.1. Healthcare Payers
4.4.2. Healthcare Providers
4.4.3. Others
4.5. By Region (In Value %)
4.5.1. North India
4.5.2. South India
4.5.3. East India
4.5.4. West India
5. India Healthcare Claims Management Market Competitive Analysis
5.1. Detailed Profiles of Major Companies
5.1.1. Wipro Limited
5.1.2. Infosys Limited
5.1.3. Tech Mahindra Limited
5.1.4. Accenture plc
5.1.5. eClinicalWorks
5.1.6. Cognizant Technology Solutions
5.1.7. Tata Consultancy Services
5.1.8. IBM India Pvt. Ltd.
5.1.9. Oracle India Pvt. Ltd.
5.1.10. Cerner Corporation
5.1.11. Allscripts Healthcare Solutions
5.1.12. McKesson Corporation
5.1.13. Optum, Inc.
5.1.14. Conifer Health Solutions
5.1.15. nThrive
5.2. Cross Comparison Parameters (Revenue, Market Share, Service Portfolio, Regional Presence, Client Base, Technological Capabilities, Strategic Initiatives, Partnerships)
5.3. Market Share Analysis
5.4. Strategic Initiatives
5.5. Mergers and Acquisitions
5.6. Investment Analysis
5.7. Venture Capital Funding
5.8. Government Grants
5.9. Private Equity Investments
6. India Healthcare Claims Management Market Regulatory Framework
6.1. Health Insurance Regulations
6.2. Data Protection Laws
6.3. Compliance Requirements
6.4. Certification Processes
7. India Healthcare Claims Management Future Market Size (In USD Mn)
7.1. Future Market Size Projections
7.2. Key Factors Driving Future Market Growth
8. India Healthcare Claims Management Future Market Segmentation
8.1. By Component (In Value %)
8.2. By Type (In Value %)
8.3. By Delivery Mode (In Value %)
8.4. By End-User (In Value %)
8.5. By Region (In Value %)
9. India Healthcare Claims Management Market Analysts Recommendations
9.1. Total Addressable Market (TAM), Serviceable Available Market (SAM), and Serviceable Obtainable Market (SOM) Analysis
9.2. Customer Cohort Analysis
9.3. Marketing Initiatives
9.4. White Space Opportunity Analysis
Disclaimer Contact UsResearch Methodology
Step 1: Identification of Key Variables
The initial phase involves constructing an ecosystem map encompassing all major stakeholders within the India Healthcare Claims Management Market. This step is underpinned by extensive desk research, utilizing a combination of secondary and proprietary databases to gather comprehensive industry-level information. The primary objective is to identify and define the critical variables that influence market dynamics.
Step 2: Market Analysis and Construction
In this phase, we compile and analyze historical data pertaining to the India Healthcare Claims Management Market. This includes assessing market penetration, the ratio of marketplaces to service providers, and the resultant revenue generation. Furthermore, an evaluation of service quality statistics is conducted to ensure the reliability and accuracy of the revenue estimates.
Step 3: Hypothesis Validation and Expert Consultation
Market hypotheses are developed and subsequently validated through computer-assisted telephone interviews (CATIs) with industry experts representing a diverse array of companies. These consultations provide valuable operational and financial insights directly from industry practitioners, which are instrumental in refining and corroborating the market data.
Step 4: Research Synthesis and Final Output
The final phase involves direct engagement with multiple healthcare claims management solution providers to acquire detailed insights into product segments, sales performance, consumer preferences, and other pertinent factors. This interaction serves to verify and complement the statistics derived from the bottom-up approach, thereby ensuring a comprehensive, accurate, and validated analysis of the India Healthcare Claims Management market.
Frequently Asked Questions
01. How big is the India Healthcare Claims Management Market?
The India healthcare claims management market was valued at USD 576 million, driven by increasing health insurance penetration and advancements in digital technologies.
02. What are the major challenges in the India Healthcare Claims Management Market?
Challenges in the India healthcare claims management market include high implementation costs, data privacy concerns, and the need for a skilled workforce to manage and operate claims management solutions. These factors hinder the widespread adoption of advanced technologies.
03. Who are the key players in the India Healthcare Claims Management Market?
Prominent players in the India healthcare claims management market include Wipro Limited, Infosys Limited, Tech Mahindra, Accenture plc, and eClinicalWorks. These companies have a significant market presence due to their extensive service portfolios, strong client relationships, and continuous innovation.
04. What factors drive the growth of the India Healthcare Claims Management Market?
The India healthcare claims management market growth is propelled by factors such as the increasing penetration of health insurance, government initiatives to promote digital healthcare, and technological advancements in claims processing systems, which streamline operations and enhance customer satisfaction.
Why Buy From Us?

What makes us stand out is that our consultants follows Robust, Refine and Result (RRR) methodology. i.e. Robust for clear definitions, approaches and sanity checking, Refine for differentiating respondents facts and opinions and Result for presenting data with story

We have set a benchmark in the industry by offering our clients with syndicated and customized market research reports featuring coverage of entire market as well as meticulous research and analyst insights.

While we don't replace traditional research, we flip the method upside down. Our dual approach of Top Bottom & Bottom Top ensures quality deliverable by not just verifying company fundamentals but also looking at the sector and macroeconomic factors.

With one step in the future, our research team constantly tries to show you the bigger picture. We help with some of the tough questions you may encounter along the way: How is the industry positioned? Best marketing channel? KPI's of competitors? By aligning every element, we help maximize success.

Our report gives you instant access to the answers and sources that other companies might choose to hide. We elaborate each steps of research methodology we have used and showcase you the sample size to earn your trust.

If you need any support, we are here! We pride ourselves on universe strength, data quality, and quick, friendly, and professional service.